Overview
Diagnosis
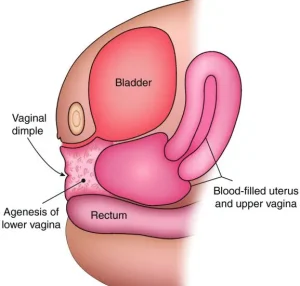
Vaginal agenesis is typically diagnosed by a pediatrician or gynecologist based on your medical history and a physical examination. The condition is often identified during puberty when menstrual periods do not start, even though breast development and pubic or underarm hair are present. In some cases, it may be discovered earlier during an evaluation for other issues or when a doctor or parent notices that a baby has no vaginal opening.
Your healthcare provider may recommend several tests to confirm the diagnosis and rule out other conditions:
-
Blood tests to check chromosome patterns and hormone levels.
-
Ultrasound to determine if you have a uterus and ovaries, and to detect any kidney abnormalities.
-
Magnetic resonance imaging (MRI) for a detailed view of your reproductive tract and kidneys.
-
Additional tests to assess hearing, heart, or skeletal development if needed.
Treatment
Treatment for vaginal agenesis usually takes place in the late teenage years or early adulthood, depending on readiness and emotional maturity. Some people may choose to delay or decline treatment, while others may pursue medical options to create a functional vagina.
Treatment options include self-dilation and surgery.
Self-dilation
Self-dilation is the first and most common approach. It allows you to create a vaginal canal without surgery. The process involves using small, rounded rods called dilators.
-
A dilator is pressed gently against the vaginal opening or inside the existing vagina for 10 to 30 minutes, one to three times per day.
-
Over time, larger dilators are used to gradually lengthen and widen the vaginal canal.
-
The process can take several months to achieve the desired result.
-
Artificial lubrication, warm baths, or switching dilator types can help ease discomfort.
-
Frequent sexual intercourse can also maintain vaginal length and function after dilation.
Some discomfort, such as bleeding or pain, may occur at the beginning. Discuss proper technique and dilator options with your healthcare provider for the best outcome.
Surgery
If self-dilation does not work, surgery to create a functional vagina (vaginoplasty) may be an option. The choice of procedure depends on your health, preferences, and the surgeon’s recommendation.
Common surgical options include:
-
Tissue graft vaginoplasty: Uses a graft from your own skin (outer thigh, buttocks, or abdomen). The graft is shaped over a mold and placed into the newly formed vaginal canal. A mold or dilator remains in place for about one week after surgery and is later used at night to maintain the canal.
-
Medical traction device (Vecchietti or balloon vaginoplasty): A small device is placed at the vaginal opening and connected to a traction system on the abdomen. Gradual tightening creates a vaginal canal over about a week. Afterward, molds or dilators are used for several months, followed by regular intercourse to maintain function.
-
Bowel vaginoplasty: Involves creating a new vagina using a small portion of the colon. This option often eliminates the need for daily dilation and provides natural lubrication during intercourse.
After any surgery, consistent use of molds, dilation, or sexual activity is necessary to maintain vaginal function. Surgical treatment is usually delayed until the individual is emotionally mature enough to manage the aftercare and follow the dilation routine, as the newly formed canal can shrink or close without maintenance.
Discuss all available options, potential risks, and aftercare requirements with your healthcare provider to determine the most suitable treatment for your needs.
Advertisement