Overview
Diagnosis
Diagnosis of genitourinary syndrome of menopause (GSM) typically involves an evaluation of your symptoms, medical history, and physical examination. Your doctor may recommend several tests to confirm the diagnosis and rule out other conditions.
Tests that may be performed include:
-
Pelvic exam: The doctor examines your pelvic organs by feeling the uterus and ovaries and visually inspecting the external genitalia, vagina, and cervix.
-
Urine test: A urine sample is collected and tested if urinary symptoms are present.
-
Acid balance test: A sample of vaginal fluids or a paper indicator strip is used to measure the acid balance (pH) of the vagina.
These tests help determine whether your symptoms are related to GSM or another medical condition.
Treatment
Treatment for genitourinary syndrome of menopause focuses on relieving discomfort and improving vaginal health. Your doctor may recommend a combination of lifestyle adjustments, nonprescription options, and prescription therapies based on the severity of your symptoms.
Over-the-counter treatment options
-
Vaginal moisturizers: Products such as K-Y Liquibeads, Replens, or Sliquid can help restore moisture to the vaginal area. Moisturizers are usually applied every few days, and their effects last longer than lubricants.
-
Water-based lubricants: Lubricants like Astroglide, K-Y Jelly, or Sliquid are applied before sexual activity to reduce discomfort. Choose products without glycerin or warming ingredients to avoid irritation. Avoid petroleum-based products if you use condoms, as petroleum can damage latex.
If these options do not provide enough relief, prescription treatments may be considered.
Topical estrogen therapy
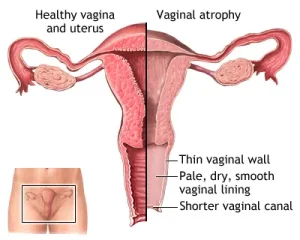
Vaginal estrogen is an effective treatment for GSM and works by restoring estrogen levels locally with minimal absorption into the bloodstream. It provides direct relief of symptoms and comes in several forms:
-
Vaginal estrogen cream (Estrace, Premarin): Applied inside the vagina with an applicator, typically daily for 1 to 3 weeks and then 1 to 3 times weekly.
-
Vaginal estrogen suppositories (Imvexxy): Inserted into the vagina daily for several weeks and then twice a week.
-
Vaginal estrogen ring (Estring, Femring): A flexible ring inserted into the vagina that releases a steady dose of estrogen for about three months.
-
Vaginal estrogen tablet (Vagifem): Inserted with a disposable applicator daily for two weeks, then twice weekly.
Oral and non-estrogen treatments
-
Ospemifene (Osphena): A daily oral medication that reduces painful intercourse caused by GSM. It is not suitable for women with a history of breast cancer or those at high risk.
-
Prasterone (Intrarosa): Vaginal inserts containing DHEA that help ease painful sex by supporting natural hormone production. Used nightly for moderate to severe vaginal atrophy.
Systemic estrogen therapy
If GSM symptoms occur alongside other menopausal symptoms such as hot flashes, systemic estrogen (in pills, patches, or gel form) may be prescribed. This treatment affects the whole body and may require the addition of progestin. Discuss the risks and benefits with your doctor before starting systemic therapy.
Vaginal dilators
Vaginal dilators can be used as a nonhormonal treatment or alongside estrogen therapy. They help stretch and stimulate vaginal muscles, improving flexibility and reducing pain during intercourse. A healthcare provider or pelvic physical therapist can teach proper use and techniques.
Topical lidocaine
Prescription ointments or gels containing lidocaine can be applied to the vaginal area 5 to 10 minutes before sexual activity to reduce discomfort.
Special considerations for women with breast cancer
If you have a history of breast cancer, treatment should be carefully coordinated with your oncologist. Options include:
-
Nonhormonal treatments: Start with vaginal moisturizers and lubricants.
-
Vaginal dilators: A nonhormonal method that can help reverse vaginal narrowing.
-
Low-dose vaginal estrogen: May be considered under medical supervision if nonhormonal options are ineffective, though there is some concern about cancer recurrence in hormonally sensitive cases.
-
Systemic estrogen therapy: Generally not recommended, especially for hormonally sensitive breast cancers.
A personalized treatment plan developed with your healthcare team will help manage symptoms safely and effectively.
Advertisement