Overview
Diagnosis
Vascular cognitive impairment is usually diagnosed based on symptoms, medical history, and evidence of blood vessel or heart-related issues. There is no single test that can confirm the condition, but several evaluations help identify its cause and severity.
Lab tests
Laboratory tests provide important information about heart and blood vessel health. These tests also help rule out other possible causes of dementia-like symptoms. Common lab evaluations may include:
-
Thyroid-stimulating hormone tests to rule out thyroid disorders
-
Blood tests to measure calcium, electrolytes, and creatinine
-
Vitamin D and vitamin B12 levels to check for deficiencies that can affect brain function
-
Blood tests for signs of infections such as syphilis, which can cause dementia in advanced stages
Neurological exam
A neurological examination helps determine how well the brain and nervous system are functioning. This exam assesses:
-
Reflexes and muscle tone
-
Strength on both sides of the body
-
Ability to walk or rise from a chair
-
Sensory responses such as touch and sight
-
Coordination and balance
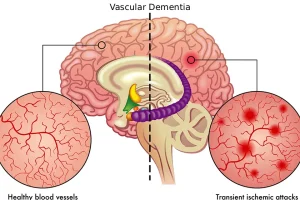
Brain imaging
Imaging studies can reveal changes in the brain caused by strokes, blood vessel disease, tumors, or trauma. These scans help identify the source of symptoms and rule out other causes.
Common imaging tests include:
-
Magnetic resonance imaging (MRI): MRI is the preferred test for diagnosing vascular cognitive impairment. It provides detailed images of strokes, mini-strokes, and blood vessel damage.
-
Computerized tomography (CT) scan: CT scans show brain structure and can detect shrinkage, stroke evidence, blood vessel changes, or tumors.
Neuropsychological tests
These tests measure how well a person can think, reason, and solve problems. They evaluate the ability to:
-
Speak, write, and understand language
-
Work with numbers
-
Learn and recall information
-
Plan and make decisions
-
Respond appropriately in different situations
People with vascular cognitive impairment often struggle more with reasoning and problem-solving than with memory loss. However, memory can still be affected if blood vessel damage impacts brain regions linked to memory.
Overlap with Alzheimer’s dementia
Vascular cognitive impairment and Alzheimer’s disease frequently occur together. Many individuals with Alzheimer’s disease also have blood vessel damage that worsens cognitive decline. Similarly, people with vascular cognitive impairment often show brain changes related to Alzheimer’s disease.
Treatment
While there is no cure for vascular cognitive impairment, treatment focuses on managing underlying conditions and preventing further brain damage. Strategies may include:
-
Controlling blood pressure, cholesterol, and blood sugar levels
-
Adopting a heart-healthy diet and regular physical activity
-
Quitting smoking and limiting alcohol use
-
Taking prescribed medications to improve blood flow and reduce stroke risk
-
Engaging in mental and social activities to support brain function
Early diagnosis and consistent management of vascular health can help slow the progression of symptoms and improve quality of life.
Advertisement