Overview
Diagnosis
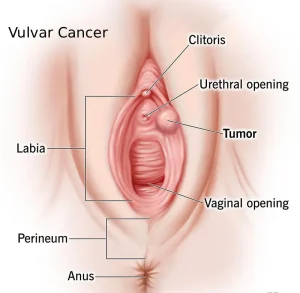
Vulvar cancer diagnosis often begins with a physical exam and a discussion of your medical history. A healthcare professional may use a special magnifying device to inspect the vulva closely, and a tissue sample may be taken for laboratory testing.
A vulvar examination is typically performed to identify any concerning areas. The healthcare provider may use a colposcope, a magnifying instrument that allows close inspection of the vulva, vagina, and cervix.
A biopsy is commonly used to confirm the diagnosis. During this procedure, a small sample of skin or tissue is removed for lab testing. Local anesthesia is used to numb the area, and a blade or circular cutting tool may be used to collect the sample. In some cases, a biopsy is done in an operating room while the patient is under sedation or general anesthesia.
If vulvar cancer is confirmed, the next step involves determining the stage of the disease. Staging helps identify how far the cancer has spread and guides treatment planning.
Staging tests may include:
-
A detailed pelvic examination to check for signs of cancer spread
-
Imaging tests such as X-ray, MRI, CT scan, or PET scan to examine the chest, abdomen, and pelvis
Vulvar cancer is categorized into four stages. Stage 1 indicates a small cancer confined to the vulva, while stage 4 represents cancer that has spread to distant parts of the body, such as the pelvic bone or other organs.
Treatment
Treatment for vulvar cancer usually begins with surgery. Other treatments may include radiation therapy, chemotherapy, targeted therapy, and immunotherapy. The treatment plan depends on factors such as the type and stage of the cancer, overall health, and patient preferences.
Surgery is often the first line of treatment and may include:
-
Wide local or radical excision: Removal of the tumor and a margin of healthy tissue around it to ensure all cancer cells are eliminated.
-
Partial or radical vulvectomy: Removal of part or all of the vulva. This procedure may be preceded by radiation or chemotherapy to shrink the tumor.
-
Sentinel lymph node biopsy: Removal and testing of a few key lymph nodes to check for cancer spread.
-
Lymph node removal: In cases where cancer has spread, multiple lymph nodes may be removed to prevent further spread.
Surgical risks include infection, delayed wound healing, and lymphedema, a condition causing leg swelling due to lymph fluid buildup.
Radiation therapy uses high-energy beams such as X-rays or protons to destroy cancer cells. It may be used before surgery to shrink tumors or after surgery to kill remaining cancer cells. Sometimes, radiation is combined with low-dose chemotherapy to enhance its effectiveness.
Chemotherapy involves powerful medicines that kill rapidly growing cancer cells. It can be administered intravenously or orally and is often combined with radiation for more advanced stages or to shrink tumors before surgery.
Targeted therapy uses drugs that attack specific molecules involved in cancer growth. By blocking these targets, the therapy helps destroy cancer cells while minimizing damage to healthy tissue. This treatment is mainly used for advanced vulvar cancer.
Immunotherapy helps the body’s immune system recognize and attack cancer cells. This therapy is considered for advanced cases when other treatments are less effective.
After completing treatment, regular follow-up exams are essential. These visits help detect any recurrence of cancer early. Typically, follow-ups are scheduled two to four times a year during the first two years after treatment.
Advertisement