Overview
Diagnosis
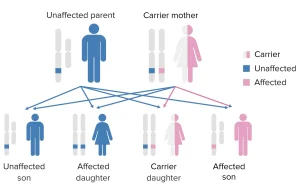
X-Linked Agammaglobulinemia (XLA), also known as Bruton’s agammaglobulinemia, is a rare genetic disorder that affects the immune system’s ability to produce antibodies. It primarily occurs in males due to mutations in the BTK (Bruton’s tyrosine kinase) gene on the X chromosome.
Diagnosis is typically made in infancy or early childhood when a child develops frequent or severe infections. The diagnostic process includes several steps:
-
Medical history and physical examination: A healthcare provider reviews recurrent infections, particularly of the ears, lungs, sinuses, and skin.
-
Blood tests:
-
Show very low or absent levels of immunoglobulins (IgG, IgA, IgM).
-
Reveal a near absence of mature B cells (identified using flow cytometry).
-
-
Genetic testing: Detects mutations in the BTK gene, confirming the diagnosis.
-
Family history review: Helps identify hereditary patterns, as the condition is passed through the maternal line.
-
Additional tests: Chest X-rays or imaging may be done to check for complications like chronic lung infections or bronchiectasis.
Treatment
Although XLA cannot be cured, treatment helps control infections and strengthens the immune response. Early and ongoing management greatly improves quality of life.
Common treatments include:
-
Immunoglobulin replacement therapy:
-
The main treatment for XLA.
-
Given intravenously (IVIG) or subcutaneously (SCIG) every few weeks.
-
Provides the body with the antibodies it cannot make on its own.
-
-
Antibiotic therapy:
-
Used to treat bacterial infections promptly.
-
In some cases, long-term low-dose antibiotics are prescribed to prevent recurring infections.
-
-
Vaccinations:
-
Live vaccines (such as MMR or oral polio) are avoided because they can cause illness in immunocompromised individuals.
-
Inactivated vaccines may be given under medical supervision, though antibody response may be weak.
-
-
Monitoring and follow-up:
-
Regular check-ups help assess lung health, sinus infections, and response to immunoglobulin therapy.
-
Lung function tests and imaging may be done to monitor for long-term damage.
-
Prevention
Since XLA is a genetic disorder, it cannot be prevented. However, steps can be taken to manage risk and support families:
-
Genetic counseling: Helps families understand inheritance patterns and assess the risk of passing the gene mutation to future children.
-
Prenatal or carrier testing: Can identify if a mother carries the BTK mutation.
-
Early diagnosis: Screening newborns with a family history of XLA allows for early treatment, reducing infection risks.
Outlook
With lifelong immunoglobulin therapy and prompt treatment of infections, most people with XLA can live relatively normal lives.
However, continuous medical care is essential to prevent chronic lung disease and other complications. Advances in gene therapy and targeted treatments are under study and may offer new hope for managing XLA in the future.
Advertisement