Overview
Diagnosis
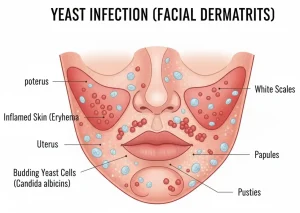
To diagnose a yeast infection on the face, a healthcare professional begins with a physical examination of the affected skin. They look for telltale signs such as redness, itching, small bumps, or flaky patches, especially in oily or moist areas like around the nose, mouth, and forehead.
If the diagnosis is unclear, additional tests may be done, such as:
-
Skin scraping or swab test, where a small sample of skin cells is collected and examined under a microscope to check for yeast growth.
-
Fungal culture, which helps identify the specific type of yeast causing the infection, most often Candida or Malassezia.
-
Patch testing, in rare cases, to rule out allergic reactions or other skin conditions that may resemble a yeast infection.
Treatment
Treatment for a facial yeast infection focuses on reducing yeast growth, easing symptoms, and preventing recurrence. The type and duration of treatment depend on the severity of the infection and the underlying cause.
Common treatment options include:
-
Topical antifungal creams or ointments, such as clotrimazole, miconazole, or ketoconazole, applied directly to the affected skin.
-
Oral antifungal medications, like fluconazole or itraconazole, for severe or widespread infections that do not respond to topical treatments.
-
Antifungal cleansers containing zinc pyrithione or selenium sulfide to reduce yeast buildup on oily skin.
-
Moisturizers and gentle skin care, avoiding heavy creams or oily products that can trap moisture and promote yeast growth.
To prevent recurrence:
-
Keep your face clean and dry, especially in humid environments.
-
Avoid using strong soaps, alcohol-based products, or steroid creams unless prescribed.
-
Manage underlying conditions such as diabetes or oily skin that may contribute to yeast overgrowth.
With proper treatment, most facial yeast infections clear up within one to two weeks. Persistent or recurrent cases may require long-term management guided by a dermatologist.
Advertisement