Overview
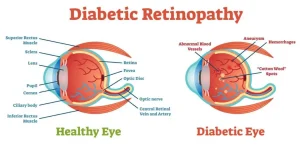
Diabetic retinopathy is a diabetes-related eye condition that damages the blood vessels of the retina, the light-sensitive tissue at the back of the eye. It develops gradually and is a leading cause of vision impairment and blindness in adults. The condition can affect people with type 1 or type 2 diabetes, especially those with long-standing or poorly controlled blood sugar levels.
Symptoms
In the early stages, diabetic retinopathy may cause no noticeable symptoms. As the condition progresses, symptoms may include:
-
Blurred or fluctuating vision
-
Dark spots or floaters in vision
-
Difficulty seeing at night
-
Impaired color vision
-
Sudden vision loss in advanced cases
-
Empty or dark areas in the field of vision
Causes
Diabetic retinopathy occurs due to prolonged damage to retinal blood vessels:
-
Chronic high blood sugar levels
-
Weakening and leakage of retinal blood vessels
-
Reduced oxygen supply to retinal tissue
-
Formation of abnormal new blood vessels
-
Inflammation and retinal swelling
Risk Factors
Several factors increase the risk of developing diabetic retinopathy:
-
Long duration of diabetes
-
Poor blood sugar control
-
High blood pressure
-
High cholesterol levels
-
Pregnancy
-
Smoking
-
Kidney disease associated with diabetes
Complications
If untreated, diabetic retinopathy can lead to serious eye problems:
-
Vision loss or blindness
-
Diabetic macular edema
-
Retinal detachment
-
Glaucoma
-
Vitreous hemorrhage
-
Permanent retinal damage
Prevention
Preventive measures focus on protecting vision and slowing disease progression:
-
Maintaining strict blood sugar control
-
Regular comprehensive eye examinations
-
Managing blood pressure and cholesterol
-
Avoiding smoking
-
Seeking prompt treatment for vision changes
-
Following recommended diabetes care plans
Advertisement