Overview
Antibiotic-associated diarrhea refers to passing loose, watery stools three or more times a day after taking medicines called antibiotics. Antibiotics are commonly used to treat bacterial infections, but they can sometimes disrupt the natural balance of bacteria in the digestive system.
About 1 in 5 people who take antibiotics experience antibiotic-associated diarrhea. In most cases, symptoms are mild and begin shortly after starting antibiotics. Mild diarrhea usually improves within a few days, either while still taking the medicine or soon after finishing the treatment.
More persistent or severe diarrhea may require stopping the antibiotic. In such cases, a healthcare professional may prescribe a different antibiotic or recommend additional treatment.
Symptoms
For many people, antibiotic-associated diarrhea causes mild symptoms that do not interfere significantly with daily activities.
Common symptoms include:
-
Loose stools
-
Passing loose stools three or more times a day
Mild symptoms may begin within hours or a few days after starting an antibiotic.
More serious symptoms can begin several days to up to two months after starting antibiotics. Severe antibiotic-associated diarrhea is often linked to infection of the large intestine, most commonly caused by a bacterium called Clostridioides difficile, also known as C. difficile or C. diff.
Symptoms of more serious diarrhea may include:
-
Frequent or severe diarrhea
-
Pain or cramping in the lower abdomen
-
Low-grade fever
-
Nausea
-
Loss of appetite
-
Dehydration
Symptoms of dehydration may include:
-
Extreme thirst or dry mouth
-
Little or no urine
-
Dark-colored urine
-
Dizziness, lightheadedness or extreme tiredness
-
Sunken cheeks or eyes
In young children, signs of dehydration may include:
-
No wet diapers for three or more hours
-
No tears when crying
-
A sunken soft spot on the head
-
Unusual drowsiness
Causes
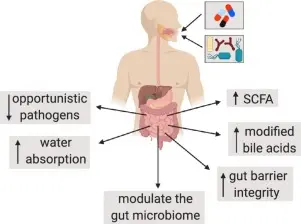
Antibiotic-associated diarrhea can occur for several reasons related to how antibiotics affect the digestive system.
Possible causes include:
-
Direct irritation or damage to the lining of the large intestine
-
Destruction of helpful bacteria that normally support digestion
-
Overgrowth of harmful bacteria, such as C. difficile, when beneficial bacteria are reduced
Nearly all antibiotics can cause antibiotic-associated diarrhea, though some are more commonly linked to it.
Antibiotics more often associated with diarrhea include:
-
Cephalosporins
-
Fluoroquinolones
-
Penicillins
-
Clindamycin
-
Carbapenems
-
Macrolides
Risk factors
Anyone who takes antibiotics can develop antibiotic-associated diarrhea, but certain factors increase the risk.
Risk factors may include:
-
A previous episode of antibiotic-associated diarrhea
-
Infancy
-
Age 65 or older
-
Long hospital stays
-
Living in a nursing home or long-term care facility
-
Having a serious underlying illness
-
Using proton pump inhibitors to reduce stomach acid
Complications
The most common complication of antibiotic-associated diarrhea is dehydration due to excessive loss of fluids and electrolytes.
Severe dehydration can be life-threatening if not treated promptly. It may cause weakness, dizziness, low blood pressure and reduced urine output. In severe cases, hospitalization may be required.
Infections caused by C. difficile can also lead to inflammation of the colon and other serious intestinal complications if left untreated.
Prevention
Several steps can help reduce the risk of antibiotic-associated diarrhea.
Preventive measures include:
-
Taking antibiotics only when prescribed and truly needed
-
Avoiding antibiotics for viral illnesses such as colds or flu
-
Washing hands frequently, especially before eating, after using the toilet and after handling garbage
-
Ensuring caregivers practice proper hand hygiene, especially in healthcare settings
-
Informing healthcare professionals about any past history of antibiotic-associated diarrhea or C. difficile infection
Sharing your medical history may allow your healthcare professional to choose an antibiotic that carries a lower risk or to monitor symptoms more closely during treatment.
Advertisement