Overview
Bedsores, also known as pressure ulcers or pressure sores, are injuries to the skin and underlying tissue caused by prolonged pressure on the skin. They commonly develop on areas of the body where bones are close to the skin, such as the heels, ankles, hips, tailbone, elbows, and shoulders. Bedsores often affect people who have limited mobility and are unable to change positions regularly.
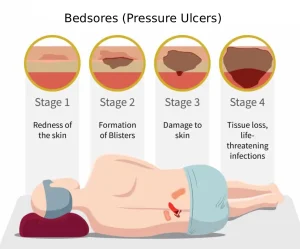
Pressure ulcers can range from mild skin redness to deep wounds that expose muscle or bone. Without proper care, they can become serious and lead to infections and other complications.
Symptoms
The symptoms of bedsores depend on their stage and severity. Early detection is important to prevent worsening.
Common symptoms include:
-
Redness or discoloration of the skin that does not fade when pressure is relieved
-
Skin that feels warmer or cooler than surrounding areas
-
Pain or tenderness in the affected area
-
Swelling or firmness of the skin
-
Blisters or open sores
-
Drainage, pus, or foul odor in advanced stages
In darker skin tones, discoloration may appear purple, blue, or ashen rather than red.
Causes
Bedsores develop due to continuous pressure that reduces blood flow to the skin and tissues. Without adequate blood supply, the affected tissue becomes damaged and may die.
Main causes include:
-
Prolonged pressure from lying or sitting in one position
-
Friction from skin rubbing against bedding or clothing
-
Shear forces when skin moves in one direction and bone moves in another
-
Moisture from sweat, urine, or stool that weakens the skin
These factors often occur together in people with limited mobility.
Risk factors
Certain conditions and situations increase the risk of developing bedsores.
Risk factors include:
-
Limited mobility due to illness, injury, or paralysis
-
Prolonged bed rest or wheelchair use
-
Poor nutrition and dehydration
-
Loss of sensation from nerve damage or spinal cord injury
-
Advanced age, as skin becomes thinner and more fragile
-
Chronic medical conditions such as diabetes or vascular disease
-
Incontinence leading to frequent skin moisture
The risk increases when preventive care is delayed or inconsistent.
Complications
If left untreated, bedsores can lead to serious health problems.
Possible complications include:
-
Skin and soft tissue infections
-
Bone and joint infections
-
Slow-healing or chronic wounds
-
Sepsis in severe cases
-
Increased pain and reduced quality of life
-
Prolonged hospital stays and higher healthcare costs
Early treatment significantly reduces the risk of these complications.
Prevention
Preventing bedsores focuses on reducing pressure, maintaining skin health, and addressing risk factors early.
Effective prevention strategies include:
-
Changing position regularly to relieve pressure
-
Using pressure-relieving mattresses, cushions, or pads
-
Keeping skin clean, dry, and moisturized
-
Inspecting skin daily for early signs of pressure damage
-
Ensuring adequate nutrition and fluid intake
-
Managing incontinence promptly
-
Encouraging movement and physical activity when possible
Consistent preventive care is essential for individuals at high risk of developing pressure ulcers.
Advertisement