Overview
Diagnosis of Alcohol Use Disorder
A healthcare professional will assess your drinking habits, overall health, and mental well-being to confirm the diagnosis.
-
Initial consultation: Most people begin with their primary care provider, who may refer them to a mental health professional for a deeper evaluation.
-
Drinking history: Your provider may ask detailed questions about how much, how often, and why you drink. With your consent, they may also speak to family or close friends for additional insight.
-
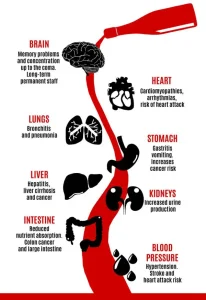
Physical examination: A physical exam can reveal visible signs of alcohol-related damage, such as liver problems or nutritional deficiencies.
-
Lab and imaging tests: While no single test diagnoses alcohol use disorder, certain lab patterns can indicate organ damage or complications related to alcohol. Imaging may be used to assess liver or other organ health.
-
Psychological evaluation: A mental health provider may conduct interviews or questionnaires to understand your emotions, behavior, and the impact alcohol has on your life.
Treatment for Alcohol Use Disorder
Treatment depends on the severity of the disorder and your individual goals. Most plans combine medical care, therapy, and lifestyle support to help reduce or stop drinking.
-
Detox and withdrawal: Medically managed detoxification (2–7 days) helps the body safely adjust to the absence of alcohol. Sedative medications may be given to manage withdrawal symptoms.
-
Developing coping skills: Alcohol treatment specialists work with you on goal setting, behavioral strategies, self-help tools, and structured recovery plans.
-
Psychological counseling: Individual, group, couples, or family therapy provides emotional support and addresses the psychological aspects of addiction.
-
Oral medications:
-
Disulfiram discourages drinking by causing unpleasant physical reactions if alcohol is consumed.
-
Naltrexone reduces cravings and blocks the pleasurable effects of alcohol.
-
Acamprosate helps maintain abstinence by managing cravings.
-
-
Injected medication: A monthly injection of Vivitrol (a form of naltrexone) can make it easier to stay on track.
-
Continuing support: Aftercare programs and support groups help with relapse prevention and long-term lifestyle changes.
-
Mental health treatment: Since alcohol use disorder often coexists with depression or anxiety, therapy and medications may be needed for both conditions.
-
Medical follow-up: Many alcohol-related health issues improve after quitting drinking, but some require ongoing care.
-
Spiritual practice: Many people find strength in spiritual or faith-based support as part of their recovery journey.
Residential Treatment Programs
For severe alcohol use disorder, inpatient rehabilitation may be recommended.
-
Comprehensive care: Residential programs typically include individual and group therapy, educational sessions, family involvement, and activity therapy.
-
Expert team: Programs often involve licensed addiction counselors, social workers, nurses, and physicians experienced in treating alcohol use disorder.
-
Structured environment: A residential setting provides a safe, supportive space to focus on recovery without daily triggers.
Prevention and Recovery Tips
-
Seek help early if you notice your drinking is increasing or becoming hard to control.
-
Build a strong support network with friends, family, and support groups.
-
Adopt healthy coping strategies like exercise, mindfulness, or hobbies.
-
Avoid triggers that encourage alcohol use.
Advertisement