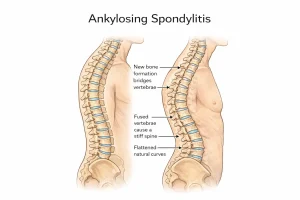
Overview
Diagnosis of Ankylosing Spondylitis
Diagnosing ankylosing spondylitis involves a combination of physical examination, imaging tests, and lab studies. Early detection can help manage symptoms effectively and prevent long-term complications.
Physical exam
During the examination, a healthcare provider may ask you to bend in different directions to check spinal mobility and flexibility. Gentle pressure on the pelvis or specific leg movements may be used to reproduce pain and identify affected joints. You may also be asked to take a deep breath to evaluate chest expansion, as reduced mobility in the rib joints is common with ankylosing spondylitis.
Imaging tests
X-rays are often the first step to detect changes in the spine and sacroiliac joints, but early disease signs may not be visible on X-rays.
MRI scans provide more detailed images of bones and soft tissues and can reveal early inflammatory changes even before structural damage occurs. Although MRI is more sensitive, it is also more expensive.
CT scans may sometimes be used for further evaluation of joint damage.
Lab tests
There are no specific blood tests to confirm ankylosing spondylitis. However, certain tests can detect inflammation markers in the blood.
Testing for the HLA-B27 gene may also be done, as its presence can support the diagnosis, but not all people with this gene develop the disease.
Treatment of Ankylosing Spondylitis
The main goals of treatment are to reduce pain and stiffness, maintain mobility, and prevent spinal deformity. Early treatment often leads to better long-term outcomes.
Medications
Nonsteroidal anti-inflammatory drugs (NSAIDs) such as naproxen sodium and ibuprofen are the most commonly used medicines to relieve inflammation and pain.
If NSAIDs are not effective, treatment may involve tumor necrosis factor (TNF) blockers, interleukin-17 (IL-17) inhibitors, or Janus kinase (JAK) inhibitors.
These medications work by controlling the immune system’s inflammatory response and are given through injections or oral tablets.
Examples of TNF blockers:
-
Adalimumab (Humira)
-
Certolizumab pegol (Cimzia)
-
Etanercept (Enbrel)
-
Golimumab (Simponi)
-
Infliximab (Remicade)
Examples of IL-17 inhibitors:
-
Secukinumab (Cosentyx)
-
Ixekizumab (Taltz)
Examples of JAK inhibitors:
-
Tofacitinib (Xeljanz)
-
Upadacitinib (Rinvoq)
Physical therapy
Physical therapy is a key component of treatment, helping to relieve pain and maintain flexibility. A physical therapist may recommend:
-
Range-of-motion and stretching exercises
-
Strengthening exercises for core and back muscles
-
Posture training and proper sleeping or walking positions
Surgery
Surgery is rarely needed but may be considered in cases of severe pain or joint damage. Hip replacement surgery may be recommended if the hip joint is severely affected.
Key Takeaways
-
Early diagnosis helps prevent long-term spinal complications.
-
Medications like NSAIDs, TNF blockers, IL-17 inhibitors, and JAK inhibitors help reduce inflammation and pain.
-
Regular physical therapy maintains flexibility and posture.
-
Surgery is an option only in severe or advanced cases.
Advertisement