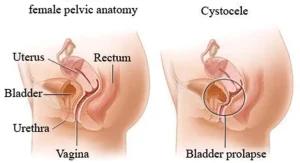
Overview
Diagnosis of Anterior Prolapse
To diagnose anterior prolapse, also known as cystocele, your healthcare professional may use several methods:
Pelvic exam
During a pelvic exam, your provider checks for tissue bulges in the vagina. You may be asked to bear down as if having a bowel movement to see how the prolapse responds. Additionally, your provider may ask you to contract your pelvic floor muscles, similar to stopping the flow of urine, to assess muscle strength.
Medical history
Your healthcare professional will review your medical and surgical history, including pregnancies and any previous pelvic issues.
Bladder and urine tests
Some patients undergo tests to check bladder function and how completely it empties. A urine sample may also be tested for infection or other abnormalities.
Treatment of Anterior Prolapse
Treatment depends on your symptoms, the severity of the prolapse, and whether you have other related conditions such as urinary incontinence or multiple pelvic organ prolapses.
Watchful waiting
If symptoms are mild or absent, no treatment may be needed. Your healthcare provider may recommend regular follow-up visits to monitor the condition.
Pelvic floor muscle exercises
Also called Kegel exercises, these strengthen the pelvic muscles to better support the bladder and pelvic organs. A physical therapist may guide you using biofeedback, which connects sensors to show if you are performing exercises correctly.
Pessary
A vaginal pessary is a silicone device inserted into the vagina to support the bladder. While it does not cure the prolapse, it can relieve symptoms. Healthcare providers will fit the device and teach you how to insert, remove, and clean it. Some patients use a pessary as a temporary solution before surgery or if surgery is not recommended.
Surgery
Surgery may be considered if other treatments do not relieve symptoms. Approaches include:
-
Vaginal surgery – The surgeon repairs the prolapse through the vagina.
-
Laparoscopic surgery – Small incisions with cameras and surgical tools may be used, sometimes with robotic assistance.
-
Open surgery – A traditional abdominal incision may be used in certain cases.
Surgical repair typically involves lifting the bladder and securing it in place.
Prolapsed uterus considerations
If anterior prolapse occurs alongside a prolapsed uterus, your healthcare provider may suggest repairing the prolapse and possibly performing a hysterectomy. Some procedures can leave the uterus in place while providing vaginal support.
Pregnancy considerations
If you are pregnant or planning a pregnancy, surgery may be postponed until after childbirth. Pelvic floor exercises or a pessary can help manage symptoms during this time.
Surgical outcomes
Results from surgery can last for many years. However, there is a risk of recurrence, which may require additional treatment or surgery in the future.
Advertisement