Overview
Diagnosis
Atrial tachycardia is diagnosed through a physical examination and by listening to your heart. During the assessment, a healthcare professional checks your blood pressure, asks about your symptoms, medical history, and lifestyle habits.
Tests to Diagnose Atrial Tachycardia
Blood tests
These tests check for conditions like thyroid disease, heart disease, or other factors that may affect your heartbeat.
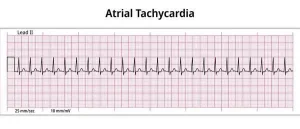
Electrocardiogram (ECG or EKG)
The most common test for diagnosing atrial tachycardia. Electrodes are placed on the chest, arms, or legs to record the heart’s electrical activity, which is displayed or printed for evaluation.
Holter monitor
A portable ECG device worn for 24–48 hours or more to record heart activity during daily activities.
Echocardiogram
Also called a heart ultrasound, this test uses sound waves to produce images of the beating heart. It shows the heart’s size, structure, and blood flow through the heart and valves.
Exercise (stress) test
Monitors heart activity during exercise, typically on a treadmill or stationary bike. If you are unable to exercise, medication may be used to mimic exercise effects on the heart.
Electrophysiological (EP) study and cardiac mapping
Performed in a hospital, this test evaluates how electrical signals travel through the heart. It helps locate the source of abnormal heart rhythms and confirms the diagnosis of atrial tachycardia.
Treatment
Treatment depends on the cause and severity of atrial tachycardia. Options include:
Vagal maneuvers
Simple actions such as coughing, placing an ice pack on the face, or bearing down (as if having a bowel movement) stimulate the vagus nerve to slow the heart rate.
Medications
Drugs may be used to control the heart rate or restore normal rhythm. Some medicines may require intravenous (IV) administration in urgent cases.
Cardioversion
A low-energy electrical shock delivered through paddles or patches on the chest to reset the heart rhythm. Used if medications or vagal maneuvers are insufficient.
Catheter ablation
A thin, flexible catheter is guided through a blood vessel, usually from the groin, to the heart. Using radiofrequency energy, tiny scars are created in heart tissue to block faulty electrical signals and restore a normal heartbeat.
Pacemaker
A small device implanted in the chest that monitors and corrects irregular heartbeats. Pacemakers are often used when other treatments fail, typically combined with AV node ablation for atrial tachycardia management.
Advertisement