Overview
Diagnosis
To diagnose dysphagia, a healthcare professional will begin by discussing your symptoms, medical history, and the nature of your swallowing difficulties. A physical examination is followed by a series of diagnostic tests to identify the underlying cause of the problem.
Common diagnostic tests include:
-
Barium X-ray: You drink a liquid called barium, which coats the lining of the esophagus, making it visible on X-rays. This test shows the shape and movement of the esophagus and can detect structural abnormalities or muscle problems. Sometimes, you may be asked to swallow solid food or a pill coated with barium to check for blockages or swallowing difficulties not visible with liquid barium.
-
Dynamic swallowing study: This involves swallowing barium-coated foods of different textures while being recorded by imaging equipment. The test reveals how well the mouth and throat muscles coordinate and whether food is entering the airway.
-
Endoscopy: A thin, flexible tube with a light and camera, called an endoscope, is passed through the throat to examine the esophagus. During this test, tissue samples (biopsies) may be taken to check for inflammation, narrowing, tumors, or eosinophilic esophagitis.
-
Fiber-optic endoscopic evaluation of swallowing (FEES): An endoscope is inserted through the nose to view the throat while swallowing. This allows for direct observation of the swallowing process.
-
Esophageal manometry: A small tube connected to a pressure sensor is placed in the esophagus to measure muscle contractions during swallowing. This test helps detect motility disorders.
-
Imaging scans: A CT scan or MRI may be used to visualize detailed structures of the throat, esophagus, and surrounding tissues. These scans help identify tumors, strictures, or neurological causes of swallowing problems.
Treatment
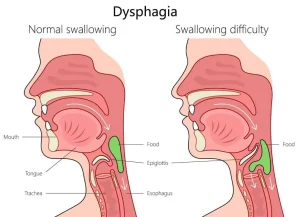
Treatment for dysphagia depends on whether it affects the throat and upper swallowing muscles (oropharyngeal dysphagia) or the esophagus (esophageal dysphagia). The goal is to restore safe and effective swallowing and address the underlying cause.
Oropharyngeal dysphagia
This type of dysphagia often results from neurological conditions and may require therapy from a speech-language pathologist. Treatment options include:
-
Swallowing exercises: Specific exercises can strengthen and coordinate the swallowing muscles or help restore nerve function.
-
Swallowing techniques: You may learn how to adjust head or body position, or modify how you place food in your mouth, to improve swallowing safety and efficiency.
These techniques are especially useful for patients with neurological disorders such as Parkinson’s disease, stroke, or Alzheimer’s disease.
Esophageal dysphagia
Treatment for esophageal dysphagia focuses on managing blockages, inflammation, or muscle disorders in the esophagus.
-
Esophageal dilation: A balloon attached to an endoscope is inflated inside the esophagus to stretch narrowed areas. It is commonly used for achalasia, strictures, or Schatzki rings.
-
Surgery: Procedures may be needed to remove tumors, correct achalasia, or treat diverticula that obstruct swallowing.
-
Medications:
-
Acid-reducing medicines help manage swallowing issues caused by GERD.
-
Corticosteroids may be prescribed for eosinophilic esophagitis.
-
Muscle relaxants may help with esophageal spasms.
-
-
Dietary management: A nutrition plan may be developed to reduce discomfort and prevent complications. For eosinophilic esophagitis, dietary changes may also serve as part of treatment.
Severe dysphagia
If swallowing is unsafe or ineffective, and nutrition cannot be maintained by mouth, a feeding tube may be required. This tube bypasses the swallowing mechanism and ensures proper nutrition and hydration.
Surgery
Certain structural or functional problems may need surgical intervention. Common surgical treatments include:
-
Laparoscopic Heller myotomy: The surgeon cuts the lower esophageal sphincter muscle to allow food to pass into the stomach more easily.
-
Peroral endoscopic myotomy (POEM): A minimally invasive alternative to Heller myotomy, performed from inside the esophagus to cut the same muscle.
-
Stent placement: A tube (stent) is inserted to keep a narrowed esophagus open. Stents may be temporary or permanent, depending on the cause.
-
Botox injection (OnabotulinumtoxinA): This relaxes the lower esophageal sphincter muscle in achalasia. It is less invasive than surgery but may require repeat treatments.
After surgery, speech and swallowing therapy is often recommended to help restore normal swallowing function.
Advertisement