Overview
Diagnosis
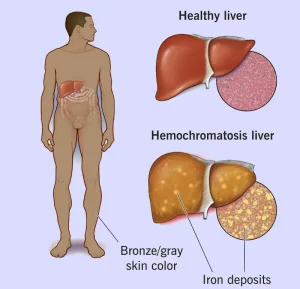
Hemochromatosis can be challenging to diagnose because its early symptoms, such as joint stiffness and fatigue, are common in many other conditions. In some cases, people have no noticeable symptoms, and the condition is discovered incidentally through routine blood tests or while screening family members of someone diagnosed with the disorder.
The primary diagnostic approach involves blood tests to measure iron levels and confirm iron overload.
-
Serum transferrin saturation: This test checks how much iron is bound to transferrin, the protein that carries iron in the blood. A transferrin saturation level above 45% is considered elevated.
-
Serum ferritin: This test measures stored iron in the liver. If transferrin saturation levels are high, ferritin is checked to confirm iron overload.
For the most accurate results, these tests are done after fasting. Because elevated levels may appear in other conditions, repeat testing is often necessary.
Additional tests may be performed to confirm the diagnosis and assess organ involvement:
-
Liver function tests: Help determine if there is any liver damage.
-
MRI: Provides a noninvasive way to measure the amount of iron in the liver.
-
Genetic testing: Detects changes in the HFE gene associated with hereditary hemochromatosis. A genetic counselor can help discuss the benefits and implications of testing.
-
Liver biopsy: In cases where liver damage is suspected, a small sample of liver tissue is taken and analyzed for iron levels and scarring (cirrhosis). Risks include bleeding, bruising, and infection.
Screening is recommended for close family members—parents, siblings, and children—of individuals diagnosed with hemochromatosis. If a gene mutation is found in only one parent, children typically do not need testing.
Treatment
Treatment for hemochromatosis focuses on reducing excess iron in the body to prevent organ damage and complications. The main approach is to remove blood regularly, which lowers iron levels naturally.
-
Phlebotomy (blood removal): The primary treatment involves removing blood from the body at regular intervals, similar to donating blood. Each session reduces iron levels because iron is used to make new red blood cells. The frequency of phlebotomy depends on the severity of iron overload and how quickly levels return to normal.
-
Chelation therapy: For individuals who cannot undergo regular blood removal due to anemia or heart problems, medicines that bind excess iron may be prescribed. These medications help the body eliminate iron through urine or stool.
-
Dietary management: Avoiding iron supplements, limiting alcohol intake, and reducing consumption of iron-rich foods such as red meat can help control iron levels.
-
Monitoring and follow-up: Regular blood tests are necessary to track ferritin and transferrin saturation levels and ensure iron remains within a healthy range.
With early diagnosis and proper management, most people with hemochromatosis can live healthy lives and avoid serious complications such as liver cirrhosis, diabetes, and heart problems.
Advertisement