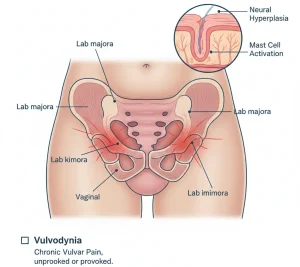
Overview
Diagnosis
To diagnose vulvodynia, your healthcare professional or gynecologist will begin by discussing your medical and sexual history, including any surgeries you may have had. The goal is to understand your symptoms and rule out other possible causes of pain or irritation.
Common diagnostic steps include:
-
Pelvic exam: Your outer genitals and vagina are checked for signs of infection or irritation. A sample of cells from your vagina may be taken to test for bacterial or yeast infections. During the exam, a gloved finger may be inserted into your vagina to check the pelvic floor muscles for tenderness or tightness.
-
Cotton swab test: A moistened cotton swab is gently touched to specific areas of your vulva to locate painful spots. You may be asked to describe what the pain feels like and how severe it is.
-
Biopsy: If the skin of your vulva looks unusual, a small tissue sample may be removed for laboratory testing.
-
Blood tests: These may be done to measure hormone levels such as estrogen, progesterone, and testosterone, which can help identify hormonal causes of pain.
These evaluations help your healthcare provider rule out infections, skin disorders, or hormonal imbalances that may be contributing to your symptoms.
Treatment
Vulvodynia treatment focuses on relieving pain and improving quality of life. Because no single treatment works for everyone, your care plan may involve a combination of medications, physical therapy, counseling, and sometimes surgery. It may take time to find the right approach, and relief can take several months.
Medications
Your healthcare provider may recommend one or more of the following:
-
Antidepressants or anticonvulsants to help reduce chronic nerve pain. Some antidepressants are available in cream form for topical use.
-
Local anesthetics such as lidocaine ointment, which can temporarily block pain. Applying it about 30 minutes before sexual activity may reduce discomfort.
-
Nerve blocks, which are injections given near specific nerves to relieve long-term pain that doesn’t respond to other treatments.
-
Hormone creams, such as estrogen or testosterone creams, if your symptoms are linked to hormonal changes.
-
Antihistamines, which can reduce itching, though they may cause dryness in postmenopausal individuals.
Therapies
Several therapeutic approaches may help relieve pain and manage symptoms:
-
Pelvic floor therapy: Exercises to stretch and relax the pelvic muscles that support the uterus, bladder, and bowel. A physical therapist may also recommend using a vaginal dilator at home to stretch and stimulate the vagina and reduce pain during sex.
-
Biofeedback: A technique that teaches you how to relax and control your pelvic muscles to reduce pain and improve muscle coordination.
-
Talk therapy: Working with a therapist can help you manage the emotional impact of chronic pain. Cognitive behavioral therapy (CBT) helps identify negative thought patterns and teaches practical coping strategies. Keeping a daily pain diary can also help track symptoms and triggers.
-
Couples or sex therapy: These therapies help partners communicate better, reduce fear of pain during sex, and build intimacy without focusing solely on sexual activity.
Surgery or other procedures
Surgery is considered only when other treatments fail and pain is localized to the tissue around the vaginal opening, known as the vestibule. The procedure, called a vestibulectomy, removes the affected tissue.
If pain affects other parts of the vulva, surgery is generally not an option. Before proceeding, your healthcare team will explain the potential benefits and risks, including the possibility of scarring or increased pain after surgery.
Vulvodynia treatment requires patience and a personalized approach. Regular follow-up with your healthcare provider ensures your treatment plan is adjusted for the best possible relief.
Advertisement